Beneath the Surface: Navigating the Landscape of Common Pelvic Floor Challenges
The pelvic floor is an intricate network of muscles, ligaments, and tissues that provides crucial support to the organs in the pelvic region. Unfortunately, many people commonly experience pelvic floor issues that can significantly impact their quality of life. In this blog post, we will delve into three prevalent pelvic floor issues: stress urinary incontinence, pelvic organ prolapse, and pelvic pain syndrome, shedding light on their causes and symptoms, and how pelvic floor PT can help you address the root cause of these impairments.
Stress Urinary Incontinence (SUI):
Stress urinary incontinence is a common pelvic floor issue that predominantly affects women, though men can also experience it. This condition involves the unintentional leakage of urine during activities that exert pressure on the bladder, such as coughing, sneezing, laughing, or exercising. The primary cause of SUI lies in the weakened pelvic floor muscles and the compromised urethral sphincter, which is responsible for controlling urine flow.
- Causes:
- Pregnancy and childbirth: The strain on the pelvic floor during pregnancy and the trauma of childbirth can lead to muscle weakness.
- Aging: Natural aging processes can result in a gradual weakening of pelvic floor muscles.
- Obesity: Excess weight can put additional stress on the pelvic floor, contributing to muscle weakening.
- Menopause: Hormonal changes during menopause can lead to a decline in muscle tone within the pelvic region.
- Overtraining: Athletes of all ages who have strong abdominal core muscles increase the pressure placed on our pelvic floor increasing strength demands to maintain continence during activities.
- Symptoms:
- Involuntary urine leakage during activities like coughing, sneezing, laughing, or exercising.
- Frequent urges to urinate.
- A feeling of incomplete bladder emptying.
- Types of Incontinence:
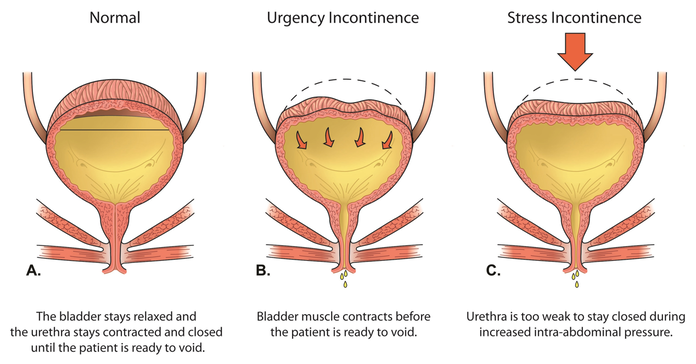
- Incontinence is classified by subtypes based on the impairment leading to your symptoms. Common types of incontinence such as stress and urge, are explained below. In some cases, these impairments overlap causing these presentations to occur in combination, such as mixed urinary incontinence.
Pelvic Organ Prolapse:
Pelvic organ prolapse occurs when the pelvic floor muscles and tissues weaken, allowing pelvic organs such as the bladder, uterus, or rectum to descend or bulge into the vaginal canal. This condition can be uncomfortable and, in severe cases, may significantly impact a person’s daily life.
- Causes:
- Childbirth: The strain of childbirth can damage pelvic floor tissues, leading to prolapse.
- Aging: As a person ages, the muscles and tissues in the pelvic region naturally weaken.
- Hysterectomy: Surgical removal of the uterus can contribute to the weakening of pelvic support structures.
- Chronic constipation: Straining during bowel movements can stress the pelvic floor.
- High Intensity / Impact Loading: With increased abdominal pressure, the pelvic floor muscles must maintain strength to adequately support these organs. Weakness in these muscles can fail against high pressures.
- Symptoms:
- A feeling of fullness or pressure in the pelvic region.
- Vaginal bulging or protrusion.
- Pain or discomfort during intercourse.
- Difficulty with bowel movements.
- Type of Pelvic Organ Prolapse:
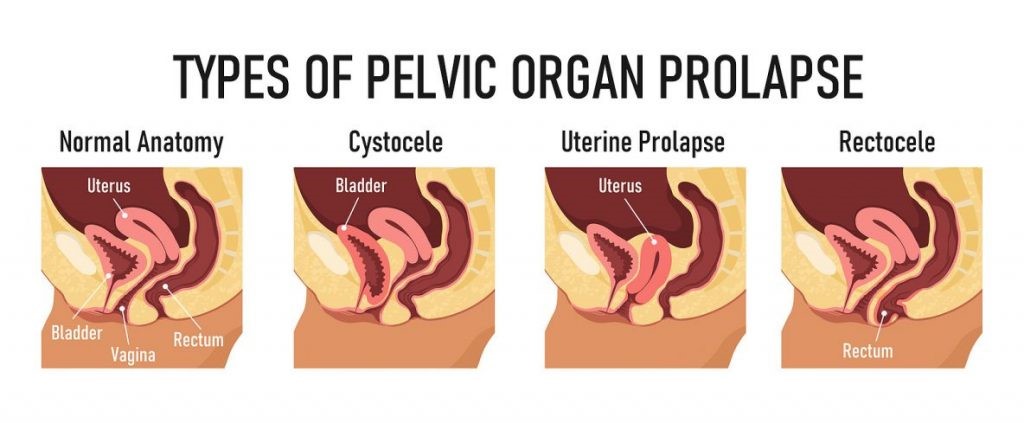
- The type of prolapse you are diagnosed with is dependent on the organ that has descended into the vaginal opening. Below is a diagram of the different anatomy within the pelvis and how this shift creates symptoms.
Pelvic Pain Syndrome:
- Pelvic pain syndrome refers to chronic, non-cyclic pain in the pelvic region that lasts for at least six months. It can affect both men and women, and its origins are often complex and multifaceted. The pain may be sharp or dull, constant or intermittent, and can have a profound impact on a person’s mental and physical well-being.
- Causes:
- Muscular issues: Tension, spasms, or weakness in pelvic floor muscles.
- Inflammation: Infections or chronic inflammatory conditions can cause pelvic pain.
- Nerve dysfunction: Irritation or compression of pelvic nerves, nervous system upregulation commonly caused by stress, anxiety, or other pain conditions.
- Trauma: Previous surgeries or injuries to the pelvic region.
- Symptoms:
- Chronic pelvic pain lasting for at least six months.
- Pain during sexual intercourse.
- Discomfort or pain while sitting.
- Frequent and urgent urination.
- Chronic Overlapping Pain Conditions:
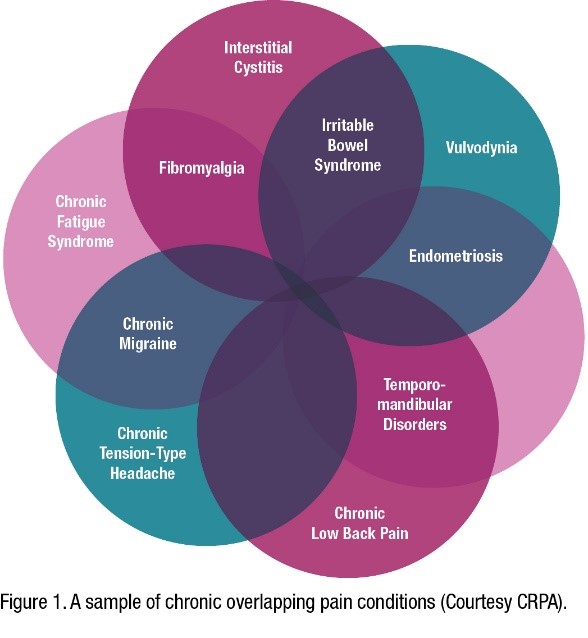
- The venn diagram to the right is a non-inclusive list of ‘chronic pain conditions’ which tend to present in overlapping occurrence. These conditions contribute to an ‘upregulated nervous system’ which creates and prolongs a stress response in our body. Due to this response, we tend to exhibit high tone in our pelvic floor muscles which contributes to pain. If you have or have been diagnosed with > 2 of these conditions and experience symptoms described above, learning how to down regulate your nervous system may help alleviate your symptoms.
Understanding common pelvic floor issues is essential for fostering awareness and seeking timely treatments. Despite many of these symptoms being widely accepted as normal consequences of aging, childbirth, and lifestyle changes, many are manageable with appropriate guidance. Whether dealing with stress urinary incontinence, pelvic organ prolapse, or pelvic pain syndrome, individuals should consult healthcare professionals to develop personalized treatment plans, including physical therapy and lifestyle modifications. By breaking the silence surrounding these issues, we can empower individuals to take control of their pelvic health and enhance their overall well-being. You should control your pelvic floor, don’t let your pelvic floor control you!
Call to book an assessment today.

