AN ATHLETE’S GUIDE TO “JUMPER’S KNEE”
What is “Jumper’s Knee” (Patellar Tendinopathy)?
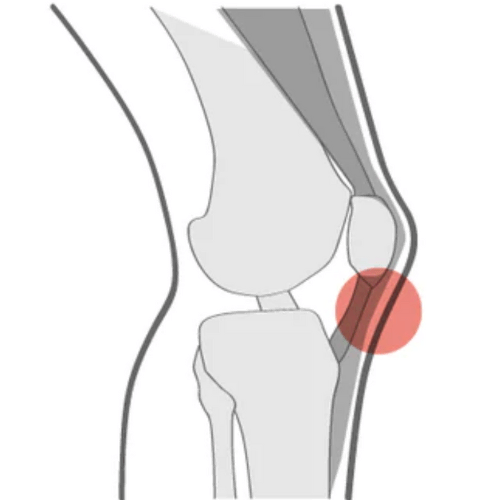
Patellar tendinopathy, also known as “jumper’s knee”, is a common injury that may develop with repetitive or unaccustomed jumping, running, squatting, or stair climbing activities. This condition presents as pain in the tendon directly inferior to the patella (kneecap) and is aggravated by activities that load the patellar tendon (Cardoso et al., 2019; Malliaris et al., 2015).
Tendinopathies often develop when there is an increase in training load or activity level to which the tendon is not tolerant to, which can cause complex cellular and structural changes within the tendon (Rio et al., 2014). Patellar tendinopathy can present at any age, regardless of sport or activity level, and can be an extremely frustrating injury to deal with.
How Do I Treat Patellar Tendinopathy?
Since tendinopathies tend to develop from an intolerance to the amount of stress being placed on the tendon, the key to rehabilitating them is to progressively load the tendon and the surrounding musculature (e.g. glutes, quadriceps, hamstrings, calves) to improve their capacity, without causing further aggravation (Malliaris et al., 2015).
It is commonly thought that rest and activity avoidance is necessary to prevent further damage and pain; however, current research has found that complete, prolonged rest is not an effective treatment strategy for tendinopathies (Cook, 2018; Malliaris et al., 2015). Rather, load management education and progressively incorporating strengthening exercises that address both the tendon itself and the entire kinetic chain, have shown to be more effective in tendinopathy rehabilitation (Malliaris et al., 2015).
How Much Is Too Much?
It is important that we are adequately stressing the tendon to ensure that we are increasing its capacity to tolerate load, while avoiding overloading it and causing an increase in pain. It can be challenging to determine the perfect happy medium and it may take some trial and error.
Typically, pain that is greater than a 4/10 during activity and pain that persists beyond 24 hours post-activity is associated with tendon overload (Kongsgaard, 2009). Therefore, it is extremely important to closely monitor pain levels during activity and in the 24 hours following activity to determine appropriate stimulus and prevent injury progression.
If the tendon does become overloaded, and pain persists for greater than 24 hours, it is important to avoid the aggravating activity for a few days to allow for adequate recovery of the tendon (Malliaris et al., 2015).
Key Takeaways
- Tendinopathy develops due to a tendon’s intolerance to the amount of stress being placed on it.
- Complete, prolonged rest is ineffective in managing patellar tendinopathy.
- Progressive strengthening of the tendon and the kinetic chain is key to improving the tendon’s capacity to tolerate load.
- Monitor pain levels during activity and in the 24 hours following activity to determine appropriate stimulus and avoid injury progression.
Tendinopathy rehabilitation can be complex and challenging. See a physiotherapist for guidance on developing a program that is tailored to you!
References
Cook, J. L. (2018). Ten treatments to avoid in patients with lower limb tendon pain. British Journal of Sports Medicine, 52(14), 882-882.
Cardoso, T. B., Pizzari, T., Kinsella, R., Hope, D., & Cook, J. L. (2019). Current trends in tendinopathy management. Best Practice & Research Clinical Rheumatology, 33(1), 122-140.
Kongsgaard, M., Kovanen, V., Aagaard, P., Doessing, S., Hansen, P., Laursen, A. H., Kaldau, N. C., Kjaer, M., & Magnusson, S. P. (2009). Corticosteroid injections, eccentric decline squat training and heavy slow resistance training in patellar tendinopathy. Scandinavian journal of medicine & science in sports, 19(6), 790–802. https://doi.org/10.1111/j.1600-0838.2009.00949.x
Malliaras, P., Cook, J., Purdam, C., & Rio, E. (2015). Patellar tendinopathy: clinical diagnosis, load management, and advice for challenging case presentations. Journal of orthopedic & sports physical therapy, 45(11), 887-898.
Rio, E., Kidgell, D., Purdam, C., Gaida, J., Moseley, G. L., Pearce, A. J., & Cook, J. (2015). Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. British journal of sports medicine, 49(19), 1277-1283.
