GEORGE’S MARVELOUS MEDICINE (FOR OSTEOARTHRITIS)
Understanding Osteoarthritis:
If 8-year-old George Kranky could concoct magic medicine that made his grandmother and various farm animals grow tens of feet tall, surely, we can formulate an antidote for osteoarthritis. However, before we begin, it is important to understand what it is that we are trying to remedy. What is osteoarthritis?
If you get started on the content below, I’ll begin collecting the ingredients needed for our magic medicine. Now, where do we keep the wine, cheese and crackers?
Arthritis affects the joints in our body. The main symptoms include joint inflammation, joint pain, swelling, stiffness, reduced range of motion and a gradual decrease in function. To help others better understand the feeling of arthritis, it was described in a creaky joints blog post as such:
“Arthritis is this constant ache that’s always in the background, like static from a radio or TV that’s always on. It never goes away but sometimes it’s easier to ignore than others. When I’m having a rough day and I’m in a lot of pain it’s the worst1”
Osteoarthritis (OA) is the most common form of arthritis. It affects more than 10% of Canadians and approximately 50% of new cases occur in those over the age of 50, as a result, it is typically defined as an age-related disorder.
The joints in our body are constantly undergoing a cycle of making new tissue and recycling old, OA is the consequence of an imbalance between this cycle of breakdown and repair. If left unmanaged, this imbalance will result in structural and functional changes to synovial joints.
Imaging of Osteoarthritis in the knee (Hunter DJ (1999)4 Fig 1).
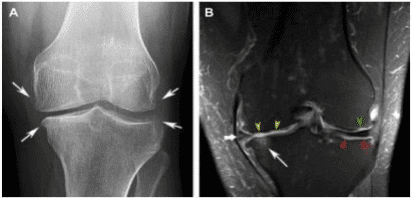
Image A: Image of a healthy knee. Notice the well-preserved joint space, contrast of the bone, healthy soft tissue (muscles), the absence of bone spurs, and bony outgrowths.
Image B: Imagine of a knee with osteoarthritis: Notice the narrowing of joint space, the presence of bony spurs along the joint and the presence of adipose (fat) in the atrophied muscles.
Rx: Magic Medicine x Osteoarthritis
Ingredient #1: Be mindful of the wording
The ultimate hyperbole of osteoarthritis is the saying bone-on-bone contact. This creates a sharp visual during movement and may create an aversive response to exercise.
The term bone-on-bone is layman’s term for joint space narrowing as a result of cartilage loss (due to the imbalance between the breakdown and repair of joint tissue).
In severe and very advanced cases of osteoarthritis, the joint space may narrow to the extent where no cartilage is left, and small areas of the bones may come in contact during certain ranges of movement. However, conservative management strategies can prevent progression to this stage of arthritis.
Ingredient #2: Understanding Pain
My favourite topic: pain science.
A common misconception is that movement is damaging because it creates pain [insert image of bone-on-bone]. Are your alarm bells turning on yet? If so, take a deep belly breath and relax. Let’s talk pain, especially hurt versus harm.
Pain does not equal tissue damage. In fact, the extent of arthritis does not equate to the amount of pain felt. There are individuals with severe OA with no pain and others with moderate OA who experience pain. A knee with osteoarthritis is a knee that is sensitized. Slight pain (3-4/10) during exercise is normal, our body can respond and adapt as long as the stresses are tolerable.
A general rule of thumb to find your tolerable level of exercise is the 24-hour rule: There should be no big increase in pain (i.e. should not increase by more than 1-2 points/10), swelling, stiffening or worsening of morning stiffness within the next 24 hours following your exercise.
Ingredient #3: Movement
There is no quick fix. The best exercise is the one you enjoy, and the recommended dosage depends on the 24-hour rule. Movement, in general, is important whether it is strength training, tai chi, yoga, aquatic exercise, cycling or neuromuscular training. Do what you enjoy and follow the 24-hour rule.
Exercise can strengthen muscles around the hip and knee, improve neuromuscular control, decreased excessive loading which will improve function and can slow the progression of arthritis.
The Role of Physiotherapy Management
The goal of OA is to be proactive instead of reactive. Physiotherapy can help prevent robust risk factors from coming into play such as obesity and joint injury. The role of physiotherapy is to guide patients to feel empowered in taking control of their own health. This can be done by movement retraining to avoid joint injury, neuromuscular and strength training, and education on topics such as pain science and joint health.
Recap:
- Osteoarthritis is a complex disorder. The medication for management is simple: redefine your pain, understand the pain and gradually add movement.
- The recommended dosage of magic medicine: Use the 24-hour rule – There should be no big increase in symptoms within 24 hours of your exercise session.
- The best exercise is the one you enjoy including but not limited to strength training, tai chi, yoga, aquatic exercise, cycling or neuromuscular training.
Fun Fact:
The GLA:D program is an evidence-based program for treatment, management and education of osteoarthritis symptoms. It is a 7-week education and exercise program for those with painful knees and hips. It is offered at Advantage Sport Medicine clinic by our very own Kacy Nishimura! For more information: contact our clinic at 780-460-9977
** Warning/Disclaimer: Do not try to make George’s marvellous medicine at home as it could be dangerous. Instead, use the medicine and prescription we recommended. It is much safer and better supported by research and clinical experience.
References:
- Arden N, Nevitt MC. 2006. Osteoarthritis: Epidemiology. Best Pract Res Clin Rheumatol 20: 3– 25.
- Garstang SV, Stitik TP. Osteoarthritis: epidemiology, risk factors, and pathophysiology. Am J Phys Med Rehabil 2006; 86(Suppl):S2-S11.
- Hunter DJ. Insights from Imaging on the Epidemiology and Pathophysiology of Osteoarthritis. Radiol Clin N Am 2009. 47:539-551.
- Knoop J et al. Improvement in upper leg muscle strength underlies beneficial effects of exercise therapy in knee osteoarthritis: secondary analysis from a randomized controlled trial. Physiotherapy, 2015. 101:171-177.
- Shane Anderson A, Loeser RF. Why is osteoarthritis an age-related disease? Best Pract Res Clin Rheumatol. 2010;24:15–26.
- https://creakyjoints.org/support/what-arthritis-really-feels-like/
- https://www.albertahealthservices.ca/findhealth/Service.aspx?id=1073354&serviceAtFacilityID=1125673
